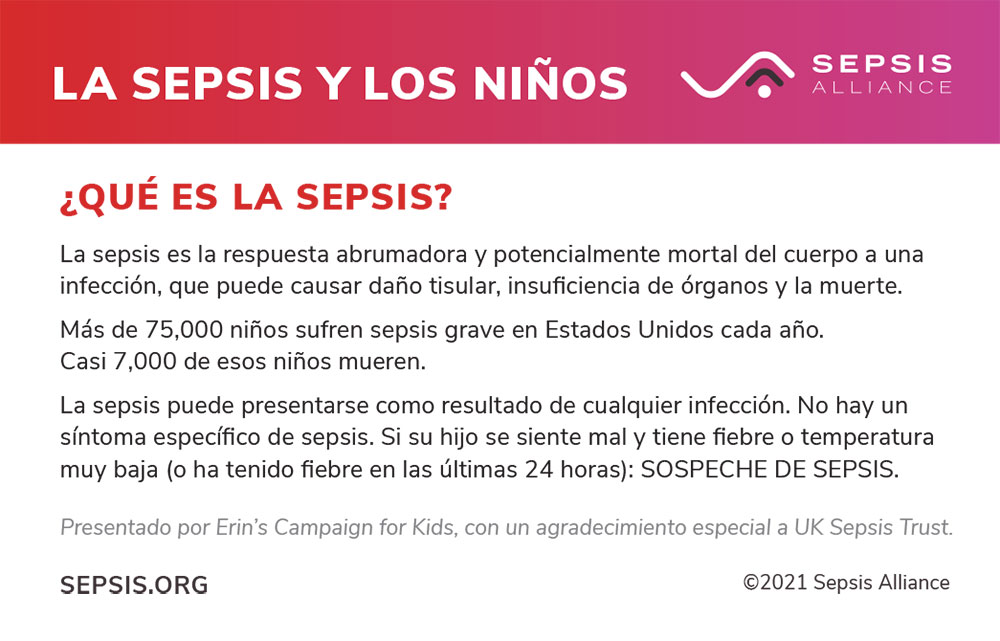
Although sepsis is the major cause of death within hospitals, up to 87% of sepsis cases originate in the community, which includes camps. Some of these infections could be:
- Infected cuts and scrapes from the playground
- Pneumonia
- Influenza
- Meningitis
- and more
Early and effective treatment reduces sepsis risk.
According to a study published in 2018, two-thirds of children in the U.S. who have severe sepsis also have an underlying chronic disease. Knowing this, professionals who work with students and campers who are compromised in any way can be aware of this increased risk. That said, although many children who are affected have an existing illness, many still have no predisposing factors for developing sepsis, yet they still get it – so awareness overall is paramount.
Sleep-away camps
Sleep-away camps also give children the opportunity to take part in activities they haven’t tried before. Outdoor activities like roasting marshmallows, kayaking, jumping in waterfalls, or rock climbing may all be new to them. Or they might be new to indoor activities, like wood working, cooking, or crafting. All these activities could cause injuries to the skin: burns, scrapes, cuts, or even blisters from walking in new shoes or hiking boots. However minor, all skin injuries are an opening for germs to enter the body and cause an infection, particularly in a camp environment that may not be as clean as at home. Take extra care to keep injuries as clean and uncontaminated as possible.
Educating camp staff
Hand washing
Washing your hands is the best defense against contracting infections, but too many people – children and adults – do not wash their hands as effectively or frequently as they should. Reminding staff about the importance of hand washing, as well as encouraging administration to make available waterless hand cleansers throughout the cabins and other buildings would likely increase compliance.
Remind campers about the importance of hand washing, and soap and water should be readily available. This simple step can help reduce the incidence of infection caused by bacterial infections, such MRSA, and viral infections, such as influenza. The summer months in North America aren’t usually associated with flu season, which tends to cover much of the school year, but the flu can be contracted year round. This infection prevention technique became even more important with COVID-19 spread around the world.
Recognizing signs of infections
Every person who works with children knows the types of injuries and illnesses that can occur. When camp counselors and other staff members are knowledgeable about basic signs and symptoms of infections, they can be the ones to draw attention to the situation.
Raising sepsis awareness in camps
Here are some ideas that may help raise sepsis awareness in camps:
Counselor and staff information sessions
Counselors and other camp staff are not nurses and are not expected to be. Arming them with sepsis knowledge could save lives though. The Sepsis 911 Information Kit, a program aimed towards the public, provides camp staff with a prepared presentation and a consistent message about what sepsis is, how it may be prevented, and how it is treated. The program is for the general public and has supporting materials for the presenters.