As children get older, their exposure to illness can increase as they attend daycare, go to school, and participate in other activities.
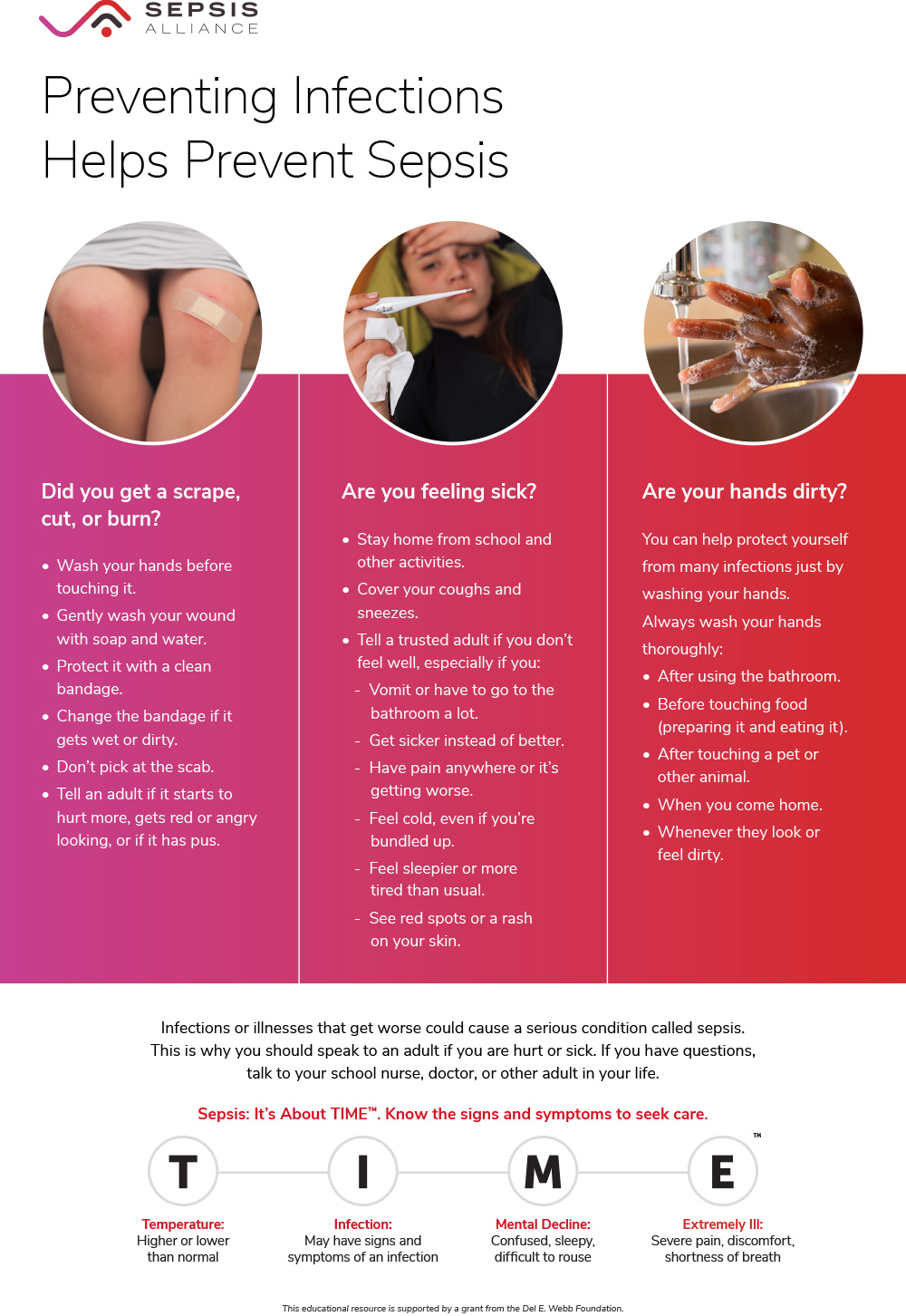
Infected wounds:
Clean any wounds properly and keep them clean. We all have bacteria on our skin, but when it gets into the wound, it could cause an infection. A common wound infection is caused by Staphylococcus bacteria, or more specifically, the one called Staphylococcus aureus (s. aureus).
Bacteria can enter the body through something as simple as a scrape on the knee or elbow, or even from a surgical incision. As superbugs, like methicillin-resistant Staphylococcus aureus (MRSA), continue to develop, there are some infections that will be much more difficult to treat than others.
Illnesses
Infections can occur in other ways as well. Children, like adults, can develop illnesses such as urinary tract infections, ear infections, pneumonia, or even meningitis. If left untreated, these can all lead to sepsis.
Symptoms
In general, signs of sepsis in children include:
- High fever (above 100.4 degrees)
- General illness or a previous injury, such as a scrape or cut
- Shortness of breath
- Very rapid heartbeat
- Drop in or no urine output
People who have survived sepsis often say that they felt the worst they ever felt in their life. For example, they had the worst sore throat of their life, the worst stomach pain, etc.
When in doubt, check with your doctor or bring your child to the emergency room for evaluation.