Septic shock is the final, most severe form of sepsis and also the most difficult to treat. Patients in septic shock are often called the “sickest patients in the hospital,” as doctors, nurses, and other healthcare professionals work to save them from long-lasting complications or death.
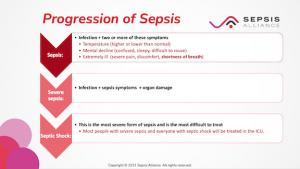
People are more likely to develop sepsis in the community than in the hospital – up to 87% of cases start from infections people contracted at work, school, or home. Sepsis can start gradually, or the symptoms can come on very suddenly. Sepsis must be treated quickly and efficiently as soon as healthcare providers suspect it. If it isn’t recognized and treated quickly, sepsis can progress to severe sepsis and then to septic shock.
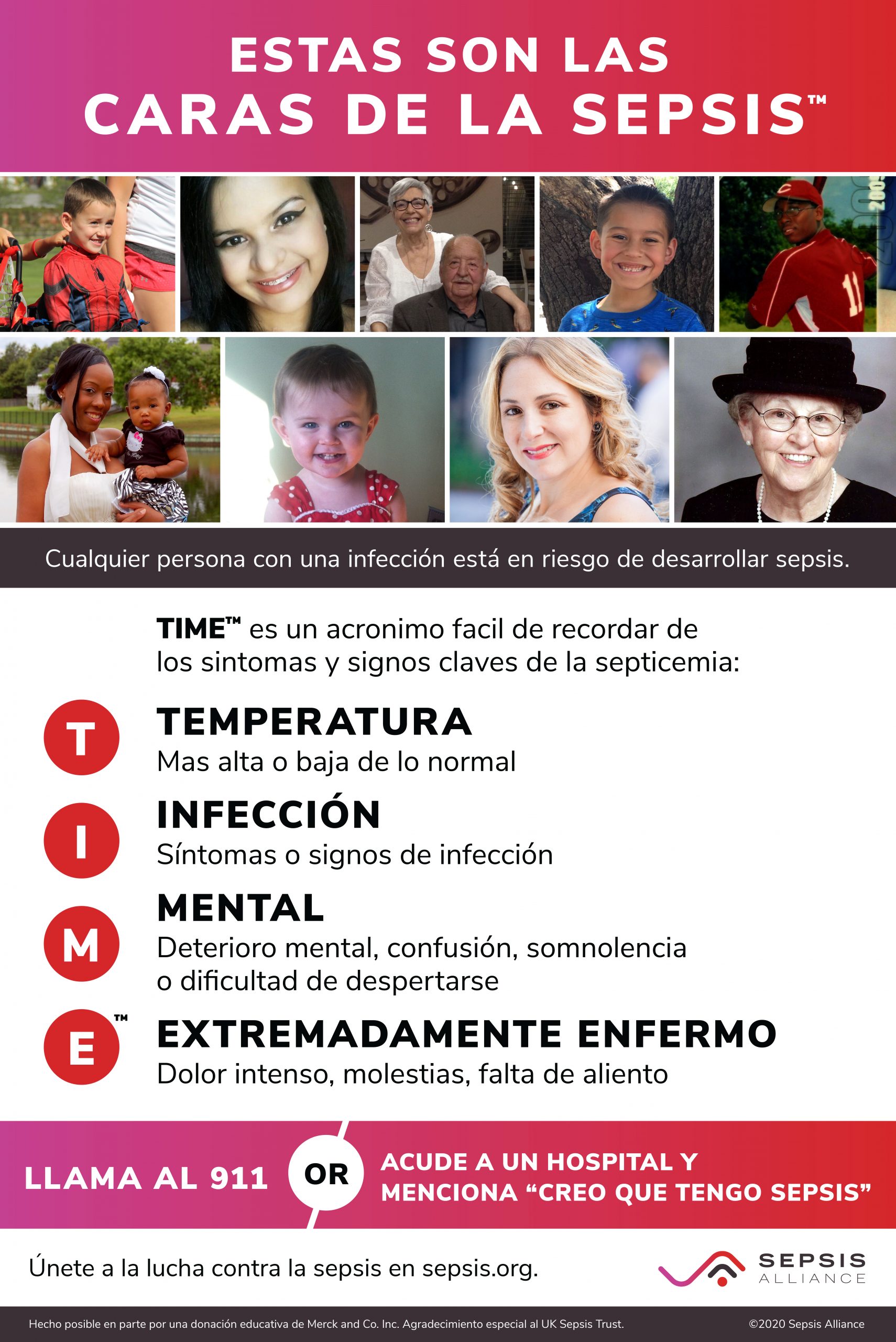
Sepsis is a life-threatening emergency that happens when your body’s response to an infection damages vital organs and, often, causes death. Like strokes or heart attacks, sepsis is a medical emergency that requires rapid diagnosis and treatment.
Suggested Citation:
Sepsis Alliance. Sepsis and Septic Shock. 2024. https://www.sepsis.org/sepsisand/septic-shock/
Updated June 18, 2024.