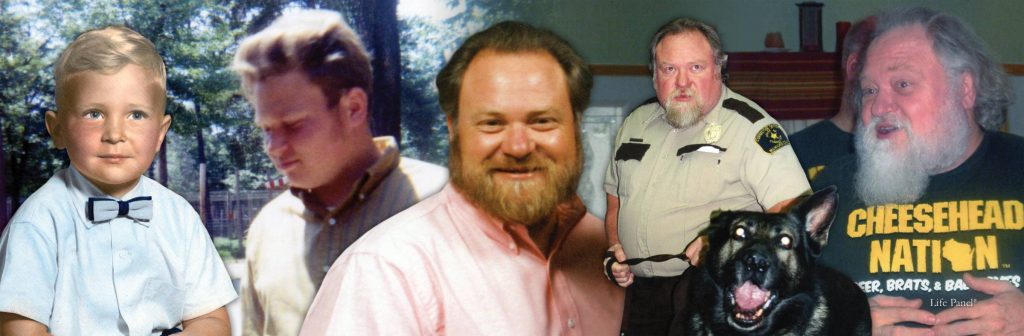
Richard Kapustanczek

My Dad was a fun-loving, sweet and gentle man who is greatly missed. I warn you now, even though this is the edited version of his story, it will be awful to read. The pain and suffering he endured is something no one should have to bear.
In February 2015, Dad was admitted in the hospital for heart-related issues. He carried 70 pounds of excess water weight. His ejection fraction (EF) rate was 20, while a normal person is 60. After 10 weeks of inpatient and nursing home stays, dad was finally discharged.
Mid-June dad went in for a follow up cardiac appointment where it was decided that he should get a defibrillator/pacemaker ICD (implantable cardiac device). At the appointment the doctor stated that without the ICD, dad would live only 1-2 years but with the ICD, 15-20 years and that the risk of infection was low.
6 weeks later on August 7th, 9-1-1 was called because Dad ‘slid out of bed’. The paramedics said he was OK after an assessment; then put him back into bed and left.
On August 8th, 9-1-1 was called again. Dad was unresponsive with an extremely low blood pressure. He was admitted into the ICU. After tests, he was diagnosed with sepsis, source unknown. By August 9th, Dad’s kidneys had shut down due to sepsis and they started dialysis. Dad spent 10 days in the ICU. The hospital said they thoroughly checked the ICD by running one test also that in 30% of sepsis cases, the source is never known. Dad spent almost 4 weeks in the hospital, receiving IV antibiotics and dialysis. We soon realized that dialysis that was not working and not having his kidneys was putting a tremendous strain on his heart. Dialysis would remove 9 pounds of excess water weight, but Dad would gain 12 pounds. It was a losing battle.
Dad was discharged from the hospital on September 1st to a skilled nursing facility for rehab and additional antibiotics. Upon admission he was 245 pounds. On September 12, he weighed 272 pounds. Every day we prayed for a miracle. My sister and I meet with the nursing home staff on September 23rd. The PT lady was upset that dad was NOT walking more. We were upset that they were not taking the MASSIVE weight gain serious. That any person could see that he was not doing well.
Dad had a follow-up cardiology appointment on September 26th. His cardiologist walked into the room and immediately picked up the phone to dial 9-1-1. Again Dad was admitted to the hospital for excessive water weight due to the heart failure and no kidney function.
Finally, Dad got a break. On October 3rd when in the hospital, Dad’s kidney functions came back. The miracle came. Dad was discharged to another skilled nursing home facility. Right around that time the antibiotic treatment ended. On October 11th, I went for my daily visit with dad and I found him half out of bed in a delirious state. The staff mentioned that he had a fever 107 degrees. I was floored that they were not doing anything about it. Finally the next day, dad was sent to the ER, sepsis again with a urinary tract infection. (Sepsis and Urinary Tract Infections) I questioned 2 doctors, ‘Are you sure it is sepsis not from the UTI and is it from the ICD pacemaker?’ Nope the catheter was pretty junky and filled with pus. This time dad didn’t lose his kidneys and only spent a few days in the ICU. Dad was discharged on October 23rd with a PICC line in his chest for IV antibiotics for the next the next 5 weeks. Dad started doing great. He was walking in PT at the nursing home. On November 11th, Dad’s ICD went off. Nothing was done by the nursing staff. I would go visit him and I could see weight gain in his legs day by day by day. When it started collecting around his waist, I asked the staff to weight him. He was 40 pounds heavier. I asked the staff if they would call his doctor. They told he if became short of breath to let them know. That’s it.
The next day on November 28th, I called all his doctors, who stated if the ICD went off he should have been taken to the ER immediately on November 15th. Dad spent another 3 weeks in the hospital. His blood cultures came clean and the PICC line was removed. Dad was discharged to his 3rd nursing home on December 11th. I met him there with his personal belongings, we chatted for a while. Monday December 12th, Dad was slow and tired. December 13th Tuesday, dad was mostly unresponsive again and stops eating. Thursday, the nursing home calls, because he is not getting up or eating, they want a psych evaluation. December 19th Dad is sent to the ER, with a fever of 103.1. They pull out the old catheter, put in a new one and the urine bag fills with pus. Dad is mostly unresponsive. On December 23rd, I hang out all day at the hospital. 4 doctors walk in, the pulmonologist, the hospitalist, the nephrologist and infectious disease doctor all state the same thing, IT HAS GOT TO BE THE PACKERMAKER AND IT NEEDS TO BE REMOVED. They also start explaining that the sepsis is pretty serious, this Staph likes to hang out on foreign bodies in the human body, like the ICD, it hangs in the pockets of spinal cord and the heart values. The electrophysiology doctor walks in; there is no conclusive evidence that it is the ICD, so the ICD stays in. The infectious disease doctor orders a nuclear white blood scan and on December 24th we get the results. There is a pocket of white blood cells near the ICD and near the base of his spine. Damn it, he was constantly complaining to the nursing staff, his lower back was hurting.
Monday December 26th, he has the ICD and the large abscess surrounding it was removed. Tuesday, they try to drain the abscess near the base of spine. They were unsuccessful in draining the abscess. Wednesday and Thursday and Friday, the EP team explains that we should put an ICD back in because he does need a pacemaker. The infectious disease doctor said no because the infection is still present the same thing will happen again. Basically us three kids, need to decide, we need to search our souls and ask the question; Our Dad WILL die, which way do we want him to die, either be massive heart attack or a slow painful death by way of sepsis. Fate decided it was the slow painful way.
Meanwhile, we can see another abscess of pus growing on his foot so what was happening on the inside of his body. Dad gets a blood transfusion on January 3rd. An EEG, shows limited brain functions. If Dad was to recover, he would not be the same person.
The hospital calls and wants a palliative care meeting on Saturday January 7th. There is no guarantee of recovery and that the treatment dad would need would be continually ICU care and don’t forget that there is no guarantee of recovery.
Sunday, we decide to put Dad in hospice and on Thursday January 12th, Dad passed at 6:12pm.
When I got the death certificate, I looked up the bacteria. This bacterium is the number one cause of cardiac device infections. Dad’s pacemaker should have been taken out in August.
After looking back at Dad’s journey, I have so many questions left unanswered. Was there ever the care out there for Dad to recover? The system failed him so many times. Between the ambulance personal who said he was OK on August 7th, to the 3 nursing homes who made no effort to speak for him or take a proactive approach with his care. SO many times, his mental status was questioned, when it was the bacteria doing the damage. I wonder what happens to the people with no advocates. Don’t get me wrong, he had some wonderful doctors and nurses and nursing assistants along the way, and I remember all their names. But other times, the staff looked like a deer in headlight when I asked questions.
It is not enough to just find a cure for sepsis. We need to make people aware of the disease and that is commonly misdiagnosed. We need to train medical personal to be advocates for their patients and require that this training be on-going. It is no longer just enough to just find a cure for sepsis. We need to change the system that allows it to happen.
We miss you every day and don’t forget to save us a spot in heaven.
Source: Jackie, Ryan and Alissa (Richard's children)






























