Maternal Sepsis and Advocating for Yourself: How I am Preparing for Birth
May 16, 2024
By Alex Sadorf Colvin, Director of Marketing and Communications
Pregnancy comes with a vulnerability that I never expected. The moment I saw two lines on a pregnancy test, my body was no longer just my own. In addition to now thinking harder about everything I eat and drink, how much I sleep, and how I work out, I am also now at the mercy of my body’s processes. This will culminate in the vulnerability of childbirth, when I must trust that I’ve picked the right doctors, the right hospital, and the right advocates to be at my side during likely the most fearful, pain-filled, and hormonally-driven moments of my life.
 I have a unique perspective after seven years at Sepsis Alliance. Most parents-to-be are not thinking about infection prevention and sepsis when making their birth plans, but for me, after the horrors I have heard from sepsis survivors and those left behind after a loss, staying sepsis safe is top of mind.
I have a unique perspective after seven years at Sepsis Alliance. Most parents-to-be are not thinking about infection prevention and sepsis when making their birth plans, but for me, after the horrors I have heard from sepsis survivors and those left behind after a loss, staying sepsis safe is top of mind.
At 25 weeks pregnant, I sat in my first educational class for parents-to-be. We went around the room to share two words we associate with “childbirth” and nearly every birthing person and their partner said some version of “nervous” or “scared” – but all in relation to pain. When I explained that my nervousness was related to complications and infections, I was met with blank stares. This isn’t surprising as only 63% of U.S. adults know the term “sepsis,” and far fewer know that sepsis/infection is the second leading cause of pregnancy-related death, causing over 261,000 maternal sepsis deaths each year worldwide. As Sepsis Alliance’s Director of Marketing and Communication, I’m too familiar with those stats.
I decided early on that I was going to do everything in my power to prevent infection in pregnancy, knowing infection prevention is sepsis prevention. Sepsis Alliance encourages everybody to learn the signs and symptoms of maternal sepsis and advocate for themselves and their loved ones. That is exactly the mindset I have brought to my pregnancy. At the time this is published, I will be 36 weeks pregnant, and here are some of the ways I have been advocating for myself and training those around me to be my advocates during my pregnancy:
I ask questions.
On my phone, I keep a running list of questions for each doctor’s appointment. From the silly first-time mom questions like, “Is it normal to feel his hiccups in my butt?” to the questions I believe everybody should be asking like, “What factors would contribute to you scheduling me for a C-section?” and “Is there anything concerning in my bloodwork that we need to watch?”
I encourage my husband to do the same, as he will be my voice during delivery and another set of eyes during the postpartum period. I need him to know what symptoms or behaviors to look out for, especially those that would lead him to take me for emergency care. One of the best ways to prepare is by asking my doctors, “What signs or symptoms should I look for, to seek emergency care?” Since working at Sepsis Alliance, I have ended many doctors’ appointments with exactly that question. Even though I know the signs and symptoms of sepsis, I want to hear from my healthcare professionals if there are any specific concerns to watch for, based on what they’ve seen of my body and experience. I encourage every person to ask this, especially birthing people and their partners when leaving the hospital.
I bring up my medical history.
I think it is important to remember that, although doctors know the body, they don’t necessarily know my body. The practice where I receive maternal healthcare probably has thousands of patients, and the doctors see multiple patients a day. Even though they have my medical chart to review before entering the room, I want to make sure they are considering the factors that make me unique when we are discussing a care plan.
My pregnancy is considered “high-risk.” In addition to being of advanced maternal age at the time of delivery (35 or older), I also have a history of deep vein thrombosis (DVT). At 25, following knee surgery, I developed a DVT behind my left knee. I have mentioned this history in every single appointment and have asked questions about how that might affect induction, epidurals, C-sections, postpartum care, and any other scenario that could come up. I have also asked how this affects my risk of infection, if at all.
I have also shared this medical history with the people who will be around postpartum. Should there be a medical emergency, I want to make sure the people closest to me know to tell any first responders of this factor, as it might affect care or test results.
I opt into prenatal care and testing.
I have opted into all genetic and prenatal testing available to me throughout my pregnancy, as well as recommended vaccines. I am also encouraging the people who will be around our newborn to get recommended vaccines such as COVID-19 boosters and Tdap (Tetanus-Diphtheria-Pertussis).
One test that gets a bad reputation, likely due to the uncomfortable nature of the test itself, is the Group B Streptococcus (GBS) test. I tested positive for GBS before pregnancy. I know the toll it takes, and the strength of the antibiotics needed to treat it. I am opting into the GBS test this week because I know that newborns are most at risk for developing severe complications and sepsis from Group B strep, and one way for my baby to develop early-onset GBS is picking it up when coming through my birth canal. Though my previous GBS diagnosis does not make me more likely to test positive again (I asked!), I will opt in to antibiotics during labor and delivery should I test positive now, to help lessen the chance of passing GBS to my infant and lower his risk of developing sepsis.
By establishing these habits, preparing myself and my husband to ask questions, bringing up my history, and watching for the signs and symptoms of infection, I can decrease my risk of maternal sepsis. These habits also establish comfort and rapport with my doctors, for me and my husband. I would love to believe I’ll be alert enough during delivery to ask my questions and take these steps on my own, but I have also prepared for that to not be the case.
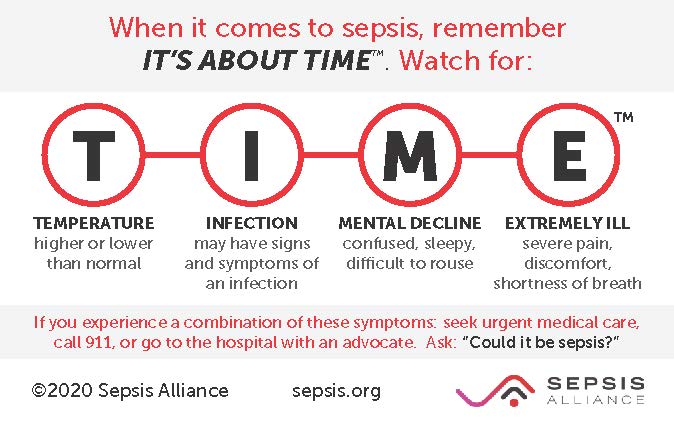
The most important question that I will teach my husband to ask is “Could it be sepsis?” If I am feeling unwell and showing any signs of sepsis, he will know to ask about sepsis explicitly. I’m going to make sure he knows the signs and symptoms, below:
Even if you aren’t pregnant, a birthing partner, or a loved one of someone soon to give birth, everybody can learn the signs and symptoms of maternal sepsis this Maternal Sepsis Week. As I mentioned above, infection prevention is sepsis prevention, and we can all do our part to lessen the risk of infection in ourselves, our loved ones, and all pregnant people.
To discover more maternal sepsis information and resources, please visit MaternalSepsisWeek.org
To send a letter to your local newspaper about the maternal sepsis crisis, please visit our Grassroots Action Center.