What is an infection?
An infection is an illness caused by germs that can make you sick. Doctors and scientists call germs microbes. Microbes are too small to see without a microscope.
There are millions of germs around you. Most don’t cause any harm. But some can if they get inside your body, where they shouldn’t be. When this happens, your immune system helps fight them. It is a defense system. Germs can cause infections anywhere in your body, like your lungs or your skin.
Most people get infections from time to time. You may feel sick or have pain while your body fights the germs. You may need to take medications. These help your immune system fight the infection. You should start to feel better once the medicines start to work.
Infections can cause a serious illness called sepsis. Instead of fighting the infection, the body starts to attack itself, the healthy cells and tissues. Sepsis can lead to severe sepsis and septic shock. Severe sepsis and septic shock can leave long-lasting health problems. They can even cause death.
What is the immune system?
The immune system helps protect you from infections. It is made up of organs, tissues, and cells all through your body, including the spleen, tonsils, bone marrow, and white blood cells.
White blood cells are proteins that fight microbes. They remember all microbes that enter the body. The white blood cells fight microbes they don’t recognize, trying to keep you from getting sick.
When the immune system doesn’t work properly
The immune system works well for most people, but not for everyone. Close to 7 million people in the United States have immune systems that don’t work well or at all, although the number could be even higher. These people can get infections more easily than they should. And they can get sicker with more severe infections.
If your immune system doesn’t work as it should, you are immunocompromised. Or you have a weakened or suppressed immune system. They mean the same thing.
Short-term and long-term weakened immune systems
Some people have a weakened immune system for just a limited time. Others live with this situation on a long-term or permanent basis.
People who have a weakened immune system for a limited time include those who:
- Receive chemotherapy, immunotherapy, or radiation for diseases like cancer.
- Take medications like steroids for a long period. Steroids treat many illnesses, like asthma, Crohn’s disease, and rheumatoid arthritis.
- Have severe burns covering a large part of the body.
- Are malnourished.
- Drink too much alcohol.
- Had a bone marrow transplant.
People who have a long-term weakened immune system include those who:
- Have no spleen, a small organ in the abdomen (belly).
- Have a disease or condition, like AIDS, diabetes, or lupus. These weaken immune responses.
- Had an organ transplant.
- Are older.
- Are very young, especially babies born too early.
 Steps you can take to protect yourself from infection
Steps you can take to protect yourself from infection
Everyone should be careful to avoid infections. Even healthy people who get infections can get sepsis. This is a serious problem. It can become septic shock.
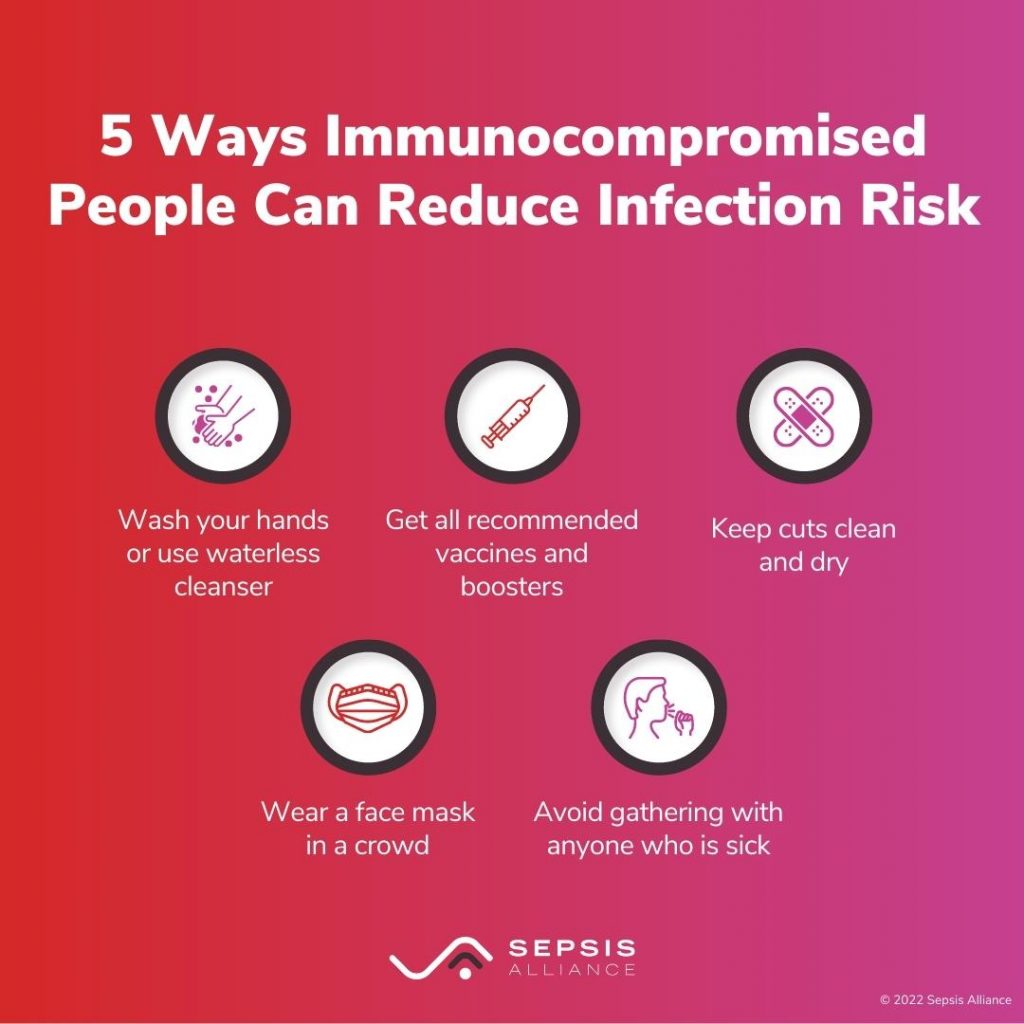
People with weakened immune systems have to be very careful. They can get infections more easily than most people. Here are some steps to help you lessen your risk of getting an infection:
- Wash your hands often. You should wash your hands with soap and water for at least 20 seconds. Don’t forget to clean under your nails and between your fingers.
- If you don’t have water, use a waterless cleanser.
- Get all vaccinations recommended by your healthcare provider. This includes the routine ones, like for measles, mumps, and rubella (MMR) and others, like for the flu, COVID-19, and pneumonia.
- Clean any breaks in your skin (scrapes, cuts, burns). Keep them clean and dry as they heal. Always wash your hands before touching a wound.
- Use antibiotic ointments on open wounds, if approved by your doctor.
- Watch for signs of infection if you have a wound. Your skin can feel warmer to touch, look red, and may have pus coming from it.
- Wear a face mask when you are in a crowd.
- Mention your immunocompromised status to all healthcare professionals you encounter. This includes not only doctors and nurses, but dentists, dental hygienists, physical therapists – anyone who provides care.
What to do if you have or suspect an infection
If you have a weakened immune system, ask your healthcare provider what you should do if you do become ill. Some doctors want their patients to call them directly. Others may tell their patients to go to an urgent care clinic or the emergency department. Being prepared can help reduce the risk of serious infections and sepsis.