Amy Levine

Although it occurred four years ago, my sepsis survival story is still a big part of who I am today, so I felt it was about time for me to share my story in honor of sepsis awareness month this year.
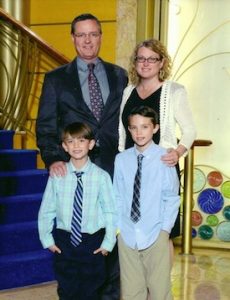
I am a wildlife conservation professional and travel to remote parts of the world a lot for work. About 10 days after my return from Vietnam four years ago, I fell ill. I remember the first day of my illness so clearly – me, my husband and two kids were at our town’s “ducky derby” and I had trouble walking along the river to follow the rubber duckies to the finish line. I was just exhausted for no good reason. That was a Saturday and I spent the next 36 hours in bed. Worried about malaria, I went to the doctor for a blood test on Monday. The results came back negative on Wednesday but by then, I was a sweaty, feverish, disoriented mess and felt like I couldn’t even sit up in bed. My husband called the doctor, who said if we were worried, we should go to the hospital. So we did.
When I arrived, my fever was over 103 and my blood pressure was 54 over 36 – dangerously low. Before completing my admissions paperwork, they rushed me into the ER, started an IV, and tilted the bed so my head was the lowest part of my body. Although I didn’t know it, I was in septic shock – but I was lucky. The ER doc recognized the symptoms as “septic appearing” immediately and the speed with which she inserted a central line and started vasopressors and fluids is probably the reason I’m alive.
 The next five days are a blur. I was admitted to the ICU where even with my head below my heart, the blood pressure alarms went off regularly for the first 24 hours. In addition to the central line, IVs in both arms allowed fluids, vasopressors, norepinephrine and seven antibiotics to course through my veins. Heparin shots every two hours minimized the chance of developing blood clots. I was in liver and kidney failure and had developed pneumonia. The doctors tested me for different bacterial and viral infections – none of which ever turned up positive, so they had no choice but to chalk the infection up as “jungle fever,” and fill my body with strong, broad spectrum antibiotics. I was so fortunate that the treatment started working. While I did have an oxygen mask, I was never intubated.
The next five days are a blur. I was admitted to the ICU where even with my head below my heart, the blood pressure alarms went off regularly for the first 24 hours. In addition to the central line, IVs in both arms allowed fluids, vasopressors, norepinephrine and seven antibiotics to course through my veins. Heparin shots every two hours minimized the chance of developing blood clots. I was in liver and kidney failure and had developed pneumonia. The doctors tested me for different bacterial and viral infections – none of which ever turned up positive, so they had no choice but to chalk the infection up as “jungle fever,” and fill my body with strong, broad spectrum antibiotics. I was so fortunate that the treatment started working. While I did have an oxygen mask, I was never intubated.
By day six, I was finally able to sit up in bed and sip a little broth. By day seven, I was moved to a step-down unit. I had not eaten in more than a week and had barely moved for seven days. I had to re-learn to walk, and could not wait to take a shower! Discharged on day 11, I didn’t feel ready to go home.
My recovery at home was slow; I didn’t feel close to normal until January. I have lasting blood pressure issues and still feel today that my cognitive abilities have been affected. Mental focus has always been hard for me, but now it’s nearly impossible. I call it my new normal. But it is only because my ER doc recognized sepsis so quickly that my family and I have the chance to experience my only slightly altered new normal. I owe my life and limbs to that doctor.
Please learn the sepsis symptoms and suspect sepsis! You could save a life like mine.


























