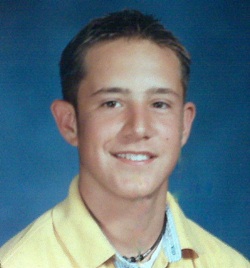
George Shearer
I stood over a hospital bed in the intensive care unit and watched over a body that I had just been told had the heart of an 80-year-old. That this heart sat inside the body of my 22-year-old son, George, left me grappling with questions, searching for answers and struggling with prayer.
Then again, George’s body hardly resembled the strong, strapping brown-eyed young man I brought into adulthood. His head had been shaven due to trauma injuries from a serious auto crash, but so much more had changed about his appearance in the 15 agonizing days since the accident.
Kidney failure had swollen his stomach and the beginning of liver failure
had turned his skin yellow. His bandaged legs hid the fact doctors had cut away so many infected layers that little was left beyond tendons and muscle. A tube jutted out of his throat, and fear filled his once beautiful brown eyes.
I told my oldest child he would be okay. I felt like such a liar, as I knew my son wasn’t okay, nor was he safe but I had to believe in hope and knew that I couldn’t let him see my fear.
After reading my son’s autopsy report; being in litigation and several depositions later, there is no doubt that a series of critical errors by doctors and nurses all along the path of my son’s ordeal led to his condition growing worse instead of better and I long to share our story not just to  make things right for George, but in the hopes of helping others avoid a similar fate. Reliving those days, however, proves challenging. Even years later, I painfully remember George closing his eyes as he went under sedation, and all the moments that followed.
make things right for George, but in the hopes of helping others avoid a similar fate. Reliving those days, however, proves challenging. Even years later, I painfully remember George closing his eyes as he went under sedation, and all the moments that followed.
I would hold his hand and whisper in his ear to let him know I was there, I would tell him how brave he is; how proud of him I am and what a wonderful son he is. I kept telling him how strong he was and that we couldn’t wait to get him back home with us. I will never forget the feeling of having his hand squeeze me back, to know that he heard me and I was reaching him.
He squeezed my hand, but he would never open his eyes again.
It began with one of those middle of the night telephone calls that seem to bring only bad news. On Jan. 24, 2006 at 4:15 a.m., I received a phone call from a hospital staffer who was located on the Florida panhandle (where my son lived at the time) to inform me they had taken him into surgery after he suffered a serious head injury in a car accident. I immediately started packing and left with my husband, Tyler, to begin the 300-mile drive across Florida. The journey that we would endure with George would be infinitely longer.
Doctors placed my son in intensive care after performing a craniotomy to relieve pressure on his brain. I was then told later after an MRI that it revealed several broken bones in his back, including the scapula, pelvic and collarbone.
In the first few days after surgery, however, George was cognizant and upbeat. Family members came by to see him, he was full of wit, telling jokes and even winning hands at playing cards. It was so encouraging seeing George in good spirits. Three days later, however, our family’s disposition began to be clouded by a series of medical staff decisions at three different facilities. A move out of intensive care, an insistence he shower, a changing of his bandaged legs while demanding he sit on a toilet in the bathroom, a transfer to a rehabilitation center in Jacksonville via my personal vehicle, and lastly failure to properly respond to a life threatening infection.
Mistake after mistake occurred despite my constant vigilance and insistence that they treat my son like they would treat their own. It started Jan. 28 at the hospital on the Florida panhandle when staff moved George from ICU to a “step-down” room that he shared with another patient – first an elderly man then a middle-aged patient with asthma. Two days 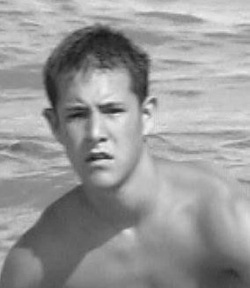 after that, one of the doctors performed a debridement, removing dead tissue from wounds on both of George’s legs. I remember George telling me he felt everything during the procedure. “If they gave me anesthesia, it didn’t work” he said. The leg pain intensified through the next day, growing so great that George constantly asked nurses for help.
after that, one of the doctors performed a debridement, removing dead tissue from wounds on both of George’s legs. I remember George telling me he felt everything during the procedure. “If they gave me anesthesia, it didn’t work” he said. The leg pain intensified through the next day, growing so great that George constantly asked nurses for help.
Then word came on Jan. 31 that the hospital wanted to transfer him to a rehabilitation center in Jacksonville (making sense because this is closer to our home). The seemingly good news got tempered, however, when the nurse insisted that George shower. George expressed grave concerns about the germs in the shower, about water entering the incision in his head from the craniotomy and his ruptured ear. The nurse would not relent, offering only that George’s grandfather could shower him if he didn’t want her to do it.
“Papa,” as George called him, helped him to the bathroom and rinsed him off. We could all hear George screaming in pain and begging to come out. My father managed to lift George out and cracked the door open to ask the nurse for help. The nurse yelled at George “shut up there are other patients on the floor”. She then said again, “just shut up and sit on the toilet, I will change the dressing on your legs here”. Despite George’s objections and begging “please don’t do this to me on a toilet, it isn’t clean in here”. Her reply again, “just shut up”.
By this time, George, my parents and I were all weeping; and it took until well into the night to calm him down. v We both prayed and cried out to God for help and I will never forget some of the most beautiful prayers I have ever heard from George as he expressed his love for Christ over and over again. We both just continued to cry together well into the night. I couldn’t believe it was only a day before we were playing cards together as he recovered from surgery.
The next morning, a hospital doctor removed the dressing on George’s legs, revealing black skin tissue tinged with a yellow/green color and a 1-inch thick red stream on the outer edges of the wounds. I asked the doctor “why is it black, that doesn’t look good”. He replied with a very stern “oh no, black is good”. Later that day, we began the transfer process for George. After making several inquiries and waiting on an answer as to when the ambulance would arrive for his transport, his doctor told me “despite having brain surgery, along with the huge leg wounds and his numerous broken bones, he can handle the drive and therefore I’m not getting him an ambulance”. I wasn’t sure how to respond; my son wasn’t supported with one splint or brace to keep his bones stable.
At that point I just wanted to get him out of there, and fast. It wasn’t long until we realized that we needed to stop and pull over in an effort to make the ride somewhat endurable. We purchased 12 king size pillows for a makeshift bed to comfort George in the back of my SUV. George’s agonizing face filled my rear-view mirror as I looked back for the majority of the trip.
I will never understand why the hospital wouldn’t arrange for an ambulance service to transfer my son even after my pleas and telling them we would pay. My son was literally broken from head to toe and was provided nothing more but a discharge sheet and a pain pill. This left us feeling totally “dismissed” as if they just wanted to wash their hands of us. Right from the beginning, officials at the rehabilitation center in our hometown appeared ill-prepared to handle a patient in George’s state. When we arrived with George at 5:15 p.m., the doctor assigned to his case already had left for the day. I called the doctor pleading “please return to evaluate George’s condition; it is obvious something is terribly wrong.” She simply told me to “hand the phone over to the nurse.” The nurse then told me she was to give George a shot of Demerol to help him get through the night.
After a sleepless and pain-filled night, a different doctor finally came the next morning to examine George. The doctor immediately appeared alarmed by the condition of George’s legs and told us “your son needs to have surgery on his legs immediately; he is at risk of losing both limbs.” I believe the doctor recognized that George had sepsis, a life-threatening bacterial infection that can lead to organ failure, but it was another 14 hours before they started administering the antibiotics needed to begin fighting this infection and 24 hours before he was scheduled for surgery for another much needed debridement of both legs.
When George arrived at the rehabilitation center the wounds were described as the following: on the left leg as being one centimeter deep, three inches wide and five inches long (3”x5”), and on the right side one and a half centimeters deep, seven inches long and five inches wide (7”x5”).
Since the time of the measurements of George’s wounds and after waiting 24 hours to clean the infection and after the surgery the measurements were now on the left lower extremity wound measured 30 centimeters (12 inches) by 15 centimeters (6 inches) by five centimeters deep (2 inches) and the right lower extremity wound measured 30 centimeters (12 inches) by 25 centimeters (10 inches) by 10 centimeters deep (4 inches).
Numbers don’t give you visual of how he had left my son’s legs. Take a ruler out take the measurements so you can get a better understanding or visual of just how much he cut away of my son’s legs because he waited so many hours while the infection continued to eat away at his legs. The surgeon expressed to us that George needed to be in ICU after this extensive surgery. I was finally feeling better about his care but after waiting to receive word from the recovery room, we later found out that he was actually transferred BACK to the rehabilitation center!!!
Even though the doctor said they would have to fight to save George’s legs and his left eye because of a similar infection, the health officials kept my son at their rehab facility for another 60 agonizing, and more importantly; avoidable hours.
The day immediately following this surgery, the facility then insisted that George needed to be seen by an off-site ophthalmologist. We were shocked as we knew George was in no condition to be at the facility – much less to leave off-site for an eye appointment! Against our concerns. The facility had EMTs transfer George to an ophthalmologist office, where he had to wait two agonizing hours on a gurney in the company of other patients for their routine exam. The EMTs were not only shocked but disgusted that George was released to go to the eye doctor instead of being seen in his room. They told me I needed to have my son transferred to ICU in an acute care facility. They expressed their concern that he was at his current facility. I begged for the EMTs to just please take my son to the hospital – but they explained this was against protocol – but they did tell me how to get him transferred.
At the advise of the EMTs, I pleaded again with the nurse when we returned to have him transferred, but to no surprise she again denied. I finally threatened to call 911 and transfer him myself (which is what the EMT said we should do) – Then, and only then, did they realize we were serious and they moved him – but not where we wanted. Unfortunately, the move was only to a regular room at the hospital. Yet again, the nightmare continued – the nurses had no clue why George was there – we had to start all over again …until they finally received his charts from the rehab facility.
I felt officially trapped in the twilight zone; a hostage and alone. I will never understand why the doctor insisted on having him stay at the rehabilitation center letting this deadly infection run ramped throughout his body and to endure the pain he went through. I trusted these people and this facility with the life of my son. Why did they make the decisions they did? It was like watching Who’s on First by Abbott and Costello only these were doctors (admitting, attending and consulting doctors) all arguing over who had responsibility for my son instead of focusing on saving his life.
Why didn’t they hear our cries for help and put my son’s life ahead of their egos?
We later learned that George was diagnosed with acute kidney failure – but only after I noticed the yellowing of his skin along with the swelling of his stomach; and when George was unable to feel his left side of his body. I had to again plead with a nurse to please come to his room and help us as she tried to insist that he just had a crick in his neck and she would look at him later! What is wrong with these people?!! I don’t understand why the staff didn’t notice he had stopped urinating. There should have been an “intake and outtake system” in place.
I stood to the side of my son, while I witnessed a male nurse insert a catheter; before my eyes I watched the bag quickly being filled with blood; and only blood…my son’s blood. I stood there feeling walls of the room closing in all around me. My knees were crumbling down as they pushed me out of the room as they worked on him as I screaming and pleading to God to save him and to George to not leave me – please George, I love you – please don’t leave me!
Wasn’t someone reading the lab work? Couldn’t they tell his kidneys were failing before they actually did?
It was then, that my son was finally transferred to ICU – after his organs started failing – not one minute before to prevent it all. It was on February 8th that the ICU nurse explained to me that my 22-year-old once vibrant son now had the heart of an 80-year-old man as he explained that George’s heart had been struggling for so many days fighting this infection that it was now damaged beyond repair.
On Feb. 9th, 16 days after the accident, we met with a doctor in the consultation room where he was explaining they were finally going to take George to surgery to remove his legs. We were told we could stop by and kiss George before they took him; but we were stopped before reaching his room. A nurse took us into the ICU waiting room and explained that George’s heart was failing and they were trying to revive him.
It wasn’t long after, the nurse returned offering only his condolences. I leaned my head on my friend’s lap and cried out, “OH NO, NOT MY SON. NOT MY SON!! NO, NO, NO. PLEASE GOD, PLEASE, PLEASE DON’T TAKE MY SON!”
I have no idea how long I said these words over and over, but I still hear my cries echo in my head and this memory always sends my heart racing. The nightmare doesn’t hit me until much later, when I finally realize it wasn’t a nightmare at all but a reality, a reality that I would never look into his deep brown eyes, hear his laugh, see him do his crazy dances in our kitchen, hear him on the phone listening to the simple words that we all take for granted, “hey, mom it’s me George”; and “I love you mom” when we hung up, and never feel the warmth of his tight hugs again.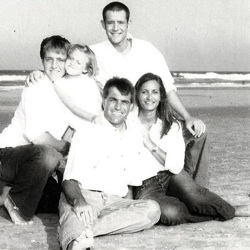
Today, those same echoes and the sweet memories of my son is where I get my strength and the passion to make a difference.
I found out after being in litigation for over the past several years that several of the surgeons and doctors that treated our son not only weren’t Board Certified, but they had failed the Board! It never even occurred to me the hospitals in Florida allowed this. This is where we are all falling under a State of False Security here.
It is my passion to, at a minimum, convenience hospitals that they should hold a higher level of care and demand that all surgeons be Board Certified if they want to practice medicine and operate at the facility. I am also hoping to have legislature pass a Bill that will mandate all hospitals, rehabilitation centers and nursing homes have a protocol in place to treat sepsis. These protocols would need to be approved by the Department of Health.
I have already become an advocate for organ donation. After noticing that George had signed his driver’s license as an organ donor; and after much soul searching, I felt called to fulfill his wish, a wish that his own organ failure took away. Therefore, I signed up as an altruistic kidney donor with the Alliance for Paired Kidney Donation. The program utilizes a unique approach in which my kidney donation, which took place on February 11th of 2010 in Birmingham, Alabama, triggered a chain of donations. The donation was made in George’s memory and is called “George’s Chain of Life.”
https://www.uabmedicine.org/kidneytransplant
https://www.parade.com/news/2011/12/the-greatest-gift.html?index=1
https://www.youtube.com/watch?v=4wQxGtRMqsc
Still, there are quiet days that I spend at George’s gravesite, sitting on his beautiful bench. I can’t tell you how many times I have cried myself to sleep there, but I have learned the true meaning and feeling of not just a broken heart, but a shattered heart. I have learned with the grace of God and my friends to put some of the pieces back together again, but my heart will never be repaired.
I hope and pray every day that he knows how much he means to me.
If anyone wants to email me (debbieshearer11@gmail.com) – please feel free to as I need all the help I can get to get these changes made so that we are no longer dealing with False Security in our Country.
Source: by Debbie Orth Shearer (George's mother)


























